Heel Pain – Plantar Fasciitis
What is it?
There are a myriad of possible causes of heel pain, from arthritis in the sub-talar joint, stress fractures in the heel bone (calcaneus), to irritation of the nerves around the heel by the wearing of hard heeled shoes. However, one of the commonest causes is known as Plantar Fasciitis, also known as heel-spur syndrome.
Plantar fasciitis presents itself as an intermittent dull pain, which may develop with time into a sharp persistent pain. Patients usually feel it at its worst in the early morning, with the first few steps of the day, or at the beginning of strenuous activity, such as sports.
What causes it?
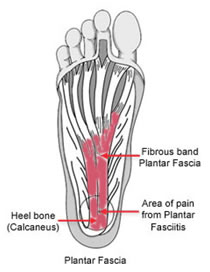
The plantar fascia is a flat band of ligament tissue that connects the bones (calcaneus) of the heel to the toes, while supporting and maintaining the arch of the foot through tension.
Problems can occur when an inflexible part of this fascia is subjected repeated bursts of tension, such as may occur in running. This repeated tension can lead to inflammation and pain, most commonly near the point where the fascia attaches to the heel bone, but can also occur in the midfoot, or nearer the toes. Due to the nature of the injury, it is difficult to rest the foot completely, so the problem tends to get worse over time.
A possible secondary result of the inflammation, that occurs in about half of all patients is the development of spike-like protrusions of new bone growth from the heel bone, known as 'heel-spurs'. At present the connection between plantar fasciitis and heel spurs is poorly understood, and it does not appear that the heel spurs themselves are the cause of pain. Some people incidentally discover heel spurs while undergoing X-rays for unrelated problems and have lived without ever feeling any heel pain.
Treatment options
The recent development of Extracorporeal Shockwave Therapy has had a transformative effect on the treatment of this condition. Whilst primary treatment of Plantar Fasciitis and other heel problems involves adjustment of activity, resting and treatment with anti-inflammatories, it is a condition that can get progressively worse. If pain is still felt after 3 months of conservative treatment and isn't eased by heel pads to reduce pressure on the plantar fascia, or lower leg splints to wear at night - then Shockwave Therapy is an excellent option.
Physiotherapy will also form part of the treatment. Click here for link to exercises for plantar fasciitis.
The best approach is one of gradual escalation from the simple to the more involved.
Improvement may take longer than expected, especially if the condition has been present for a long time. During recovery, loss of excess weight, good shoes and keeping weight off your feet all help the injury to heal. Even after the pain has gone, you should return to full activity gradually.
Rest - Use pain as your guide. If your foot is too painful, rest it.
Ice - The pain is acused by inflammation sore applying a plastic bag of crushed ice or frozen peas as soon as you feel symptoms developing often helps
Medication - Anti-inflammatory/analgesic medication (in tablet form), combined with heel pads may be all that is necessary to relieve pain and reduce inflammation. If no pain relief has occurred after two or three months, however, an injection of either cortisone and/or local anaesthetic directly into the tender area may be considered.
Physiotherapy - The objective of physiotherapy (when needed) is to decrease the inflammation. Later, the small muscles of the foot can be strengthened to support the weakened plantar fascia.
Click here for link to exercises for plantar fasciitis.
Plantar fascia specific exercises have also been shown to improve outcome for patients with chronic heel pain.
Heel Pads - A heel pad of felt, sponge or a newer synthetic/gel material can help to spread, equalise and absorb the shock as your heel lands, thus easing the pressure on the plantar fascia.
Shoes & Inserts - Poorly fitting shoes can cause plantar fasciitis. The best type of shoe to wear is a good running shoe (jogger/trainer) with excellent support. Orthoses are special shoe inserts that can be tried.
Taping - Taping your foot to maintain the arch may benefit some people as this can take some of the pressure off the plantar fascia.
Night Splints - These are splints that keep the foot stretched and the ankle at right-angles when you are asleep. This maintains the tension in the plantar fascia and may help to alleviate some early-morning symptoms during the first few steps of the day. Use of these may also improve the condition over some weeks (although there are no good studies demonstrating conclusively they are of long-term benefit patients have found them very helpful). The Strassburg Sock is probably the most confortable night splint to wear as it is less bulky than the plastic splints available.

Extracorporeal Shock Wave Therapy – A relatively new treatment, ESWT uses high intensity sonic waves that can be focused precisely deep inside the inflammed tissues. The treatment is simple, quick and non-invasive in that it does not require injections etc.
The equipment resembles and Ultrasound Scanner, but produces far more powerful waves strong enough to create 'bubble cavitation' at the focus point. The effect of this on the surrounding tissue is to reduce inflammation. It has also been found that the treatment promotes the production of growth factors and new blood vessels, which aid in the healing process. Further information on ESWT.
Surgery - Surgery is rarely required for plantar fasciitis and is best approached when conservative avenues have been exhausted and if the pain is still troublesome after at least 12 months of treatment. The surgery entails releasing the plantar and fascia and a small nerve through a 3 cm incision on the side of the foot.
Prognosis
Ligaments heal and repair themselves slowly, so recovery from Plantar Fasciitis can take longer than expected, depending on the severity and progression of the condition. A full recovery will be possible, but due to the aggravating nature of physical activity, a slow return to form is advised. To maintain fitness during this period, particularly cardiovascular fitness, weight bearing sports (jogging, running) should be replaced with non weight-bearing ones (swimming, cycling etc.)
For further information, see http://www.patient.co.uk/health/plantar-fasciitis-leaflet