Hallux Valgus (Bunions)
Modern Hallux Valgus Treatment – Operate Early
Historically, surgery for bunions (Hallux Valgus) had a less than encouraging reputation. The outcomes of surgery were often poor, due to frequent recurrence of the deformity and symptoms combined with severe post operative pain and a long recovery. This led to doctors and relatives recommending a "do nothing" approach.
Hallux Valgus and bunions are common with a prevalence of 23% in adults aged 18-65 years and 35.7% in patients aged over 65 years. Prevalence increases with age and is higher in females.
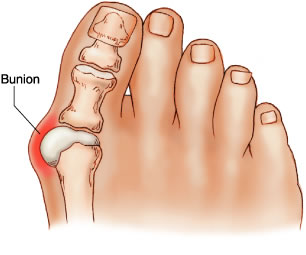
The cause is thought to be a genetic predisposition with an imbalance of intrinsic and extrinsic forces on the joint. Tight footwear and high heels exacerbated this tendency. This imbalance causes varus deviation of the metatarsal with valgus deviation of the toe and this exposes the bunion prominence. The prominence is made up of the bony 'shoulder' of the metatarsal and thickened overlying soft-tissues (capsule/bursa/skin). It is associated with a number of conditions that cause soft-tissue laxity, such as Rheumatoid Arthritis.
Presentation is usually due to pain or increasing deformity. The pain can come from the bunion prominence, from the joint due to arthritic changes or due to effects on the lesser toes (transfer metatarsalgia and hammer toe deformity).
The results of modern surgery are substantially better, with published satisfaction rates of 94% (Adam 2011). This improvement is due to advances in surgical techniques, with the modern types of osteotomy and screw fixation providing a more stable construct. This reduces the surgical pain and allows immediate weightbearing. New techniques provide more precise bony realignment and balancing of the soft-tissues, with greatly improved immediate and long-term corrections. The latest advances in minimally invasive surgery further reduce surgical trauma, infection rates and recovery times.
The surgery is performed routinely as a daycase, under anaesthesia with a regional anaesthetic (ankle block) for pain relief. The patients are discharged the same day, fully weightbearing in a protective shoe. No plastercast is necessary. They have improved recovery, reduced pain, immediate weightbearing and early return to work.
Surgery is rarely essential and more accommodative shoeware should be tried first. Unfortunately, toe-spacers, braces and orthotics do not help in the long term. Custom made shoes can be very good for severe cases where surgery is contra-indicated.
The timing of surgery and when to recommend it is a common quandary. In a stable situation, when there has been no change in deformity or symptoms, wider more accommodative shoes can help. In an unstable situation, when the pain or deformity is increasing or there are changes to the lesser toes (clawing or metatarsalgia), surgery should be considered. If left, the deformities will get worse, making surgery more complex and more extensive and previous studies have shown that surgery in these cases do less well, with higher complications and recurrence rates.

Conventional Hallux Valgus surgery. Severe bunion pre-op on left and post-op result on right.

Minimally Invasive Surgery for less severe bunion at 2 weeks post-op.