Calcaneal Fractures

Calcaneal fractures are severe injuries – those involving the main body of the heel bone and the subtalar joint, distinct from smaller peripheral fractures. They will often cause long lasting symptoms and as such, require careful assessment with appropriate imaging and a tailored surgical plan when indicated.
The surgery is complex with higher risks than other fractures – the correct management is essential to reduce these risks.
Initial Presentation
These fractures most commonly occur after a high-energy impact, such as a fall from a height onto hard ground or a road-traffic collision. There is usually extensive swelling and bruising, which will persist for many months regardless of the treatment pathway.
Investigation
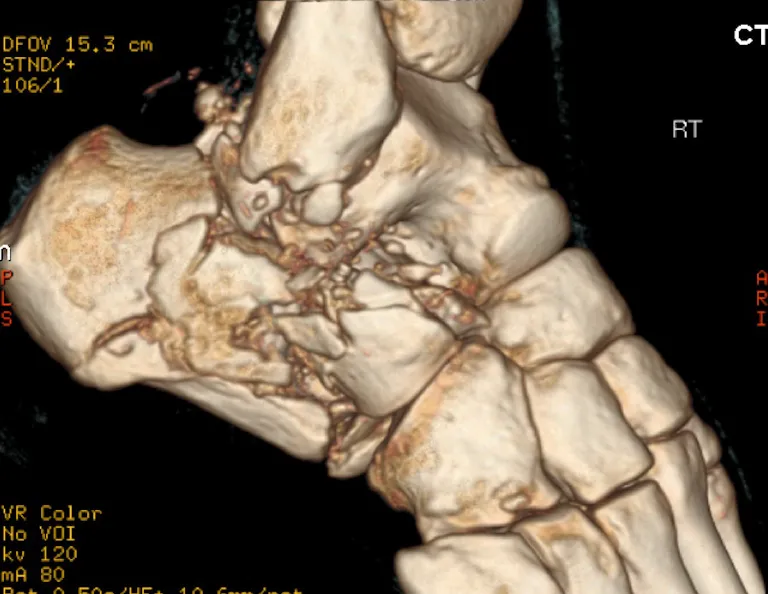
Standard X-rays of this bone can be hard to interpret and may miss the fracture or under-represent the extent of the injury.

A CT scan is essential to accurately evaluate:
- The degree of articular involvement
- The number of fracture fragments
- Joint displacement
- Overall fracture morphology
The CT will identify the severity of the injury and whether surgery is indicated or not.

Note. There is also a high incidence of peroneal tendon dislocation with these injuries, which is frequently missed without careful assessment.
How bad is it?
Severity is determined on the CT by:
- The number of fracture fragments
- The degree of joint displacement
- Sanders classification on CT
Less severe fracture types:
No or minimal displacement and the subtalar joint has minimal disruption. The number of fragments is less important.
Severity increases with:
Number of fragments and increasingly displaced. Greater disruption to the subtalar joint. Disruption of the calcaneocuboid joint.

When Is Surgery Required?
Surgery is not indicated for undisplaced or minimally displaced fractures.
Surgery is indicated for displaced intra-articular fractures, to restore joint alignment thereby minimising the risk of arthritis developing later.
The specific technique depends on the fracture pattern.
Options include:
- Open fixation
- Arthroscopic fixation
- Percutaneous (minimally invasive) fixation
- Primary subtalar fusion for severely comminuted patterns
Management of Displaced Fractures
Open Surgery
Open reduction may be required for certain multi-fragmentary or severely displaced patterns. Surgery can only be safely performed once acute swelling has improved, typically 2–3 weeks after injury.
Two main approaches are used:
Extended lateral (L-shaped) incision:
Large incision on the outside of the heel. Provides excellent exposure but carries a higher risk of wound complications. Uses a specific and large plate to secure the fragments.

Sinus tarsi incision:
Smaller incision on the outside of the heel. Provides a more limited exposure but significantly reduced soft-tissue risks, and therefore commonly preferred. Fixation is with a specific sinus tarsi plate.
Post-operative Course
- Immobilisation in a plastercast for 2-6 weeks
- Non-weight bearing for 4-6 weeks
- Full weight bearing from 6 weeks onwards
- Physiotherapy and rehabilitation can start once the wounds are well healed – usually after 3-4 weeks.
Arthroscopic Calcaneal Fixation
Arthroscopic fixation is a minimally invasive technique that I developed and have used at the Imperial Major Trauma Centre for over 15 years.
This method combines:
- Percutaneous fracture reduction
- Arthroscopic visualisation of the subtalar joint
- Precise restoration of the joint surface under direct vision
Key advantages include:
- Minimal soft-tissue trauma
- Ability to operate immediately, without waiting for swelling to subside
- Lowest infection risk of all approaches
- Rapid wound healing
- Early physiotherapy, typically from 1 week post-operatively
- No plaster cast required
This technique is particularly beneficial in displaced 2-part or 3-part fractures where joint surface accuracy is critical.
REFERENCE
Percutaneous Arthroscopic Calcaneal Osteosynthesis: A Minimally Invasive Technique for Displaced Intra-Articular Calcaneal Fractures
Philip S. Pastides, MRCS, MSc (Orth Eng), MBBS, BSc (Hons) ∙ Peter F. Rosenfeld, FRCS (Orth) ∙ Lydia Milnes, MRCS


Post-operative Course
- Immobilisation in a protective orthopaedic boot
- Physiotherapy starts at 1 week
- Non-weight bearing for 4 weeks
- Light weight bearing during weeks 4–6
- Full weight bearing from 6 weeks onwards
Most patients return to normal daily activities by 10–12 weeks, though swelling and discomfort may persist. Light sporting activity is typically possible from 16 weeks.
Risks
Key risks associated with calcaneal fracture surgery include:
- Infection (significantly lower with minimally invasive techniques)
- Wound-healing complications, particularly with extended lateral approaches
- Nerve injury, especially involving the sural nerve. More common in open surgery.
- Joint stiffness, especially of the subtalar joint (common and expected)
- Post-traumatic arthritis, which may require future interventions including subtalar fusion
Long-Term Outcomes
Even with optimal treatment and rehabilitation, some residual symptoms are common. Most patients achieve good function, including participation in recreational sport, but mild long-term stiffness or activity-related discomfort can occur. Outcomes are generally favourable, although some variability is expected due to the nature of the injury.
Even in cases where the fracture is severe and there are significant problems despite surgery, excellent salvage options are available. Either management with targeted steroid injections or with further surgery - Subtalar fusion (Subtalar Arthrodesis). This fusion provides reliable long term pain relief and restores high levels of function, including return to sport.
Severe Multi-fragmentary Fractures
These injuries have poor outcomes with standard surgical techniques, often with continued disabling pain and stiffness. These frequently require later subtalar fusion over the next 2-5 years.

My preferred surgical solution is an acute or primary subtalar fusion. I perform this procedure arthroscopically, reducing wound complications and improving recovery profiles. In my experience, the results have been very positive with patients returning relatively rapidly to their previous levels of daily function.

This is a particularly specialised area and the decision requires detailed CT review and discussion with your surgeon, regarding the expected outcomes.
I have written an article for OrthOracle that describes this technique in detail and reflects my current approach to managing severe calcaneal fractures.
REFERENCE
Calcaneal fracture: Primary arthroscopic subtalar fusion
Orthoracle