Triple Fusion
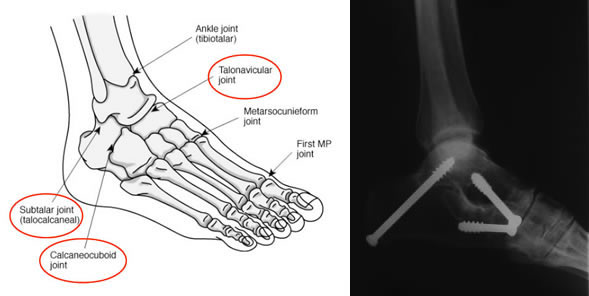
The triple joints are the Subtalar, Calcaneocuboid and Talonavicular joints, they are separate to the ankle (up/down movement). They are involved in the flexibility and movements of the foot particularly on uneven ground, whereas most of the up / down movements are at the ankle above.
A triple arthrodesis consists of the surgical fusion of the talocalcaneal (TC), talonavicular (TN), and calcaneocuboid (CC) joints in the foot. The primary goals of a triple arthrodesis are to relieve pain from arthritic, deformed, or unstable joints.
This operation removes the degenerate joints and fixes the joints together, with the aim that bone will grow across and 'fuse' the joints. The joints will then be rigid and no longer painful. This significantly reduces the normal movement, although this has usually already been lost due to the arthritis. Walking on flat ground will be almost unaltered, but walking on uneven ground will be the most apparent. Driving will be unaffected.
The surgery is performed through two 7cm incisions either side of the hindfoot and ankle. The arthritic joint surfaces are excised (cut out) and the joints fixed together with screws. The operation takes approximately 2 hours.
Risks of surgery
Swelling
Initially the foot will be very swollen and needs elevating. The swelling will disperse over the following weeks & months but will still be apparent at 6-9 months.
Infection
This is the biggest risk with this type of surgery. You will be given intravenous antibiotics to prevent against it. The best way to reduce the chance of acquiring an infection is to keep the foot elevated for 14 days. If there is a mild infection, it often resolves with oral antibiotics. If the infection is severe, it may warrant admission to hospital and intravenous antibiotics. A severe infection often results in failure of the fusion, and extremely rarely may result in an amputation at a later date.
Malposition
Ideally, the fusions are performed in a position that allows optimum function and gives the best appearance. I take great efforts to judge the best position at surgery, but as you are asleep and lying down, it is not always possible to achieve this 'best'; position. If the position is not optimal following surgery, most deformities can be accommodated by insoles and shoeware. Rarely is further surgery required.
Non Union
This is when the joint fails to fuse and bone has not grown across the joint. We won't know whether this is the case for 6-12 months. The risk of this is approximately 5%. Smoking increases this risk 16 times.
If a non union does occur and is painful, then further surgery is usually needed.
Nerve Damage
Alongside the incisions are three nerves – the superficial peroneal, sural and saphenous nerves. They supply sensation to the sides and the top of the foot and toes. They may become damaged during the surgery and this will leave a patch of numbness, either at the side of the foot or over the top of the foot and toes. This numbness may be temporary or permanent. There is approximately a 10-15% of this happening.
Recovery from surgery
After surgery, your leg will be immobilised in a backslab (half plaster) for 2 weeks. Elevation of the foot (above the pelvis) for the first 10 days is vitally important to prevent infection. Naturally, small periods of walking and standing are necessary, but no weight must be taken through this leg for 6 weeks.
After 2 weeks the backslab will be removed and the stitches taken out, here in clinic. Another non-weight bearing plaster is applied for a further 4 weeks. At this stage you will be reviewed in clinic with x-rays and changed to a weight bearing plaster for a further 6 weeks.
You will be reviewed again at 3 months following surgery, with x-rays. If all is well, no more plaster casts are needed and you can walk freely. Usually no physiotherapy is required. If the fusion is slow to heal, then a further 6 weeks in a weight bearing cast will be necessary.
Activity and time off work
In general, up to 4 weeks off work is required for sedentary posts. 12 weeks for standing or walking posts. 16 weeks for manual / labour intensive posts.
Follow up
- 2 weeks for removal of sutures & Change Of Plaster
- 6 weeks in Mr Rosenfeld's clinic - COP to WB cast / AP & Lateral X-rays
- 3 Months for Removal of POP / X-ray Ankle WB AP & Lateral Xray / Mobilise FWB out of POP
- 6 months for final assessment if no complications